The Human Microbiome: Beyond Digestive Health
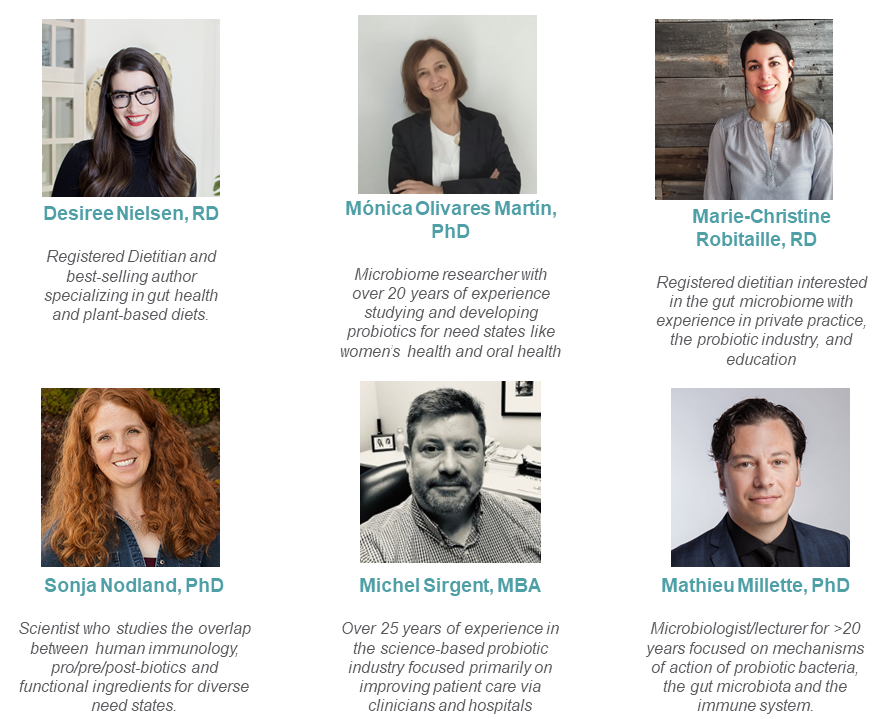
Did you know that there are just as many or more bacterial cells residing in or on our body as human cells? These microbes make up our microbiome play a large role in health, and they don’t only live in our gut or digestive tract. They live on our skin, in our mouth, and many more places and can even communicate with body systems they are not actively living in, like our brain or immune system.
As a result, while most people think about digestive health or gut health when they hear the word “microbiome”, its effects reach far beyond our digestive tract. These effects include areas of health like mood, dental health, or even exercise. On this page, our microbiome experts focus on the microbiome’s role beyond digestive health.
What is the microbiome?
The human microbiome refers to the trillions of microorganisms that reside on the skin, mouth, digestive tract, and many other body sites. These microorganisms are increasingly understood for affecting metabolism as well as our immune and nervous systems. The presence of certain microorganisms in our microbiome are known to be good for us, while others are either associated with or known to cause harm. For example, some beneficial intestinal microorganisms can breakdown fibers that are otherwise non-digestible and convert them into short chain fatty acids. These fatty acids can be used by our colonic tissues for energy and also prime the immune system towards a healthy equilibrium. Other microorganisms that are more associated with harm, produce endotoxin, a compound that causes inflammation. Our knowledge of the composition and balance of the microbes residing in the human microbiome, as well as the resultant impacts on health, is rapidly expanding.
On this page:
This page primarily focuses on how the microbiome can influence our health outside of digestive health. The resources below are helpful to learn more about the microbiome’s role in digestive health.
Learn more about the gut microbiome:
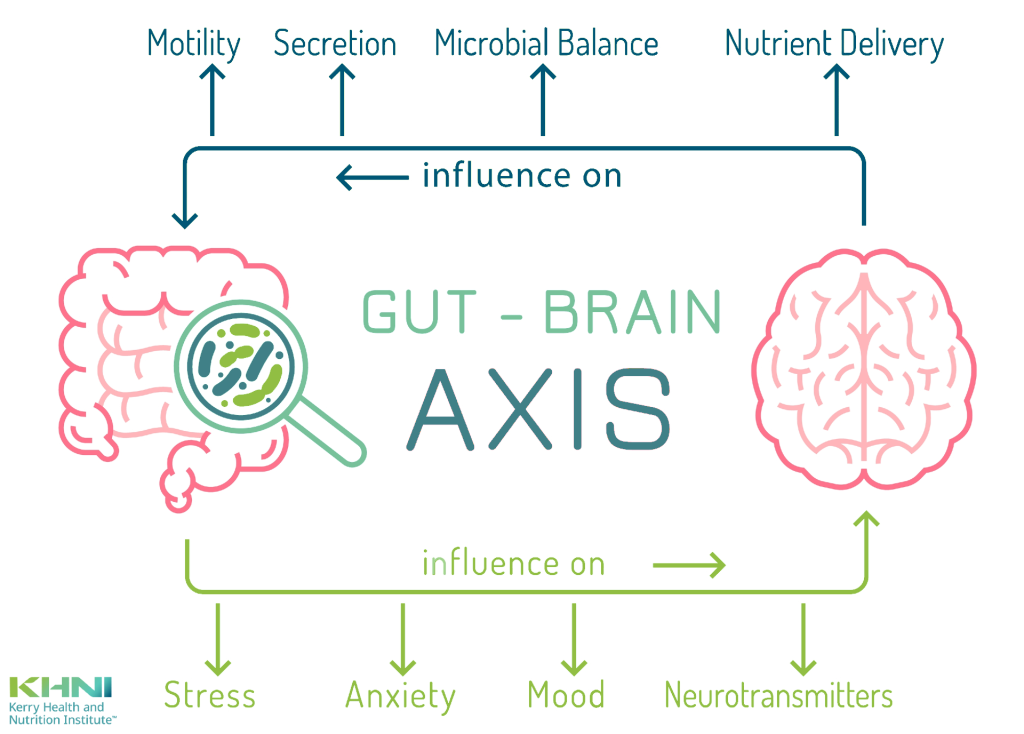
Our microbiome experts
We leveraged a wide range of experts in microbiology, probiotic research, and nutrition to build a comprehensive, science-based resource on the ever-evolving microbiome space.
The Skin Microbiome
What is the skin microbiome?

Just like our insides (like our gastrointestinal system) are protected by microbiota (friendly or ‘commensal’ microorganisms) so too is our epidermis (skin). We’ve all heard the phrase ‘it made my skin crawl’-or something to that effect. Well, in fact, our skin is literally crawling with microscopic orgasms including microbes, viruses and even some mites. According to Drs. Elizabeth Grice & Julia Segre (2011), the microbiota on our skin would be more diverse and more subject to change over time than even the microbes in our mucosal membranes (respiratory, digestive and urogenital tracts).
Why is the skin microbiome important?
Skin is often referred to as the body’s first line of defense, but our skin microbiome may act as our skin’s first line of defense by supporting barrier function to keep harmful bacteria off of the skin or out of the body.
Grice and Segre postulate that ‘dysregulation of skin immunity’, presumably from a lack of friendly defenders on our skin, is linked to skin problems such as atopic dermatitis, chronic skin wounds and acne, to name but a few. Almost 10 years after Grice & Segre, Paula Caroline Luna states that this dynamic bacterial ecosystem must constantly to change and evolve so it can continue to play its “skin barrier function”. This too suggests that the skin as a ‘barrier’ is only as good as the microbes on it.
In the case of acne, for example, it has been proposed that bacteria such as Cutibacterium acnes, Malassezia species, or even Candida species residing on the skin may be a causative factor. Modulation of the skin microbiome to make it harder for these species to colonize on the skin is one area of current study.
|
Get KHNI articles delivered to your inbox
|
Skin conditions however, can lead to more systemic conditions as is case with a staph (Staphylococca) infection, where staphylococcus aureus (most commonly) enters the bloodstream though a wound or cut in the skin and can cause sepsis (blood poisoning). It’s possible that an abundance of staph on one’s skin may be the result of insufficient friendly microbes with which they would have to compete.
Additional reading: The Skin and Gut Microbiome and Its Role in Common Dermatologic Conditions
The Oral Microbiome
 The oral microbiome is one of the most diverse and complex microbial communities in the human body, including bacteria, fungi, viruses, and protozoa. The diversity reflects the wide range of nutrients and microorganisms that enter our body the mouth through foods and drinks.
The oral microbiome is one of the most diverse and complex microbial communities in the human body, including bacteria, fungi, viruses, and protozoa. The diversity reflects the wide range of nutrients and microorganisms that enter our body the mouth through foods and drinks.
Oral bacteria are organized in structures known as biofilm, a three-dimensional ecosystem composed of a variety of microorganisms, extracellular polysaccharides, proteins and lipids and cell fragments. It is a very complex structure which provide protection and resistance to the penetration of external agents.
Why is the oral microbiome important?
Caries and periodontal diseases may be caused by harmful bacteria, such as Streptococcus mutans, Actinomycetes or Prevotella species adhering to teeth and producing acid, leading to caries. The excessive metabolic activity of these bacterial groups produce acid from fermentable carbohydrates, and lead to a localized chemical dissolution of the tooth. On the other hand, tooth-associated oral microbiome dysbiosis can stimulate the immune system leading to an inflammatory response resulting in periodontal destruction and bone resorption.
Changes in the composition and function of the oral microbiome may alter host-microbiome interaction with consequences for oral health but also for general health. The alteration of this fine equilibrium leads to dysbiosis allowing growth or colonization of opportunistic pathogens.
Oral dysbiosis does not just affect to oral health, multiple systems including the cardiovascular, digestive, endocrine and others are involved. Endocarditis, diabetes, rheumatoid arthritis, and Alzheimer’s disease have been related to periodontal disease.
What influences the oral microbiome?
There are diverse factors affecting microbiome conformation. The most known factor is the diet. It is well known that a high sugar diet provides a favorable environment for caries associated bacteria, thereby increasing the prevalence of the disease. Smoking also affects the composition of oral microbiome and the effects can even persist for years after quitting. The use of antibiotics also induces changes in oral microbiome. Other changes are related with physiological conditions, for example, hormonal factors during pregnancy favor oral microbiome dysbiosis increasing the risk or worsening of caries or periodontal disease. So, it is recommended for women to take special attention to their oral health during pregnancy period.
Learn more:
-
- Oral Microbiome, Oral Health and Systemic Health: A Multidirectional Link
- Oral microbiome findings challenge dentistry dogma
- The Oral Microbiota: Community Composition, Influencing Factors, Pathogenesis, and Interventions
- Impact of Oral Microbiome in Periodontal Health and Periodontitis: A Critical Review on Prevention and Treatment
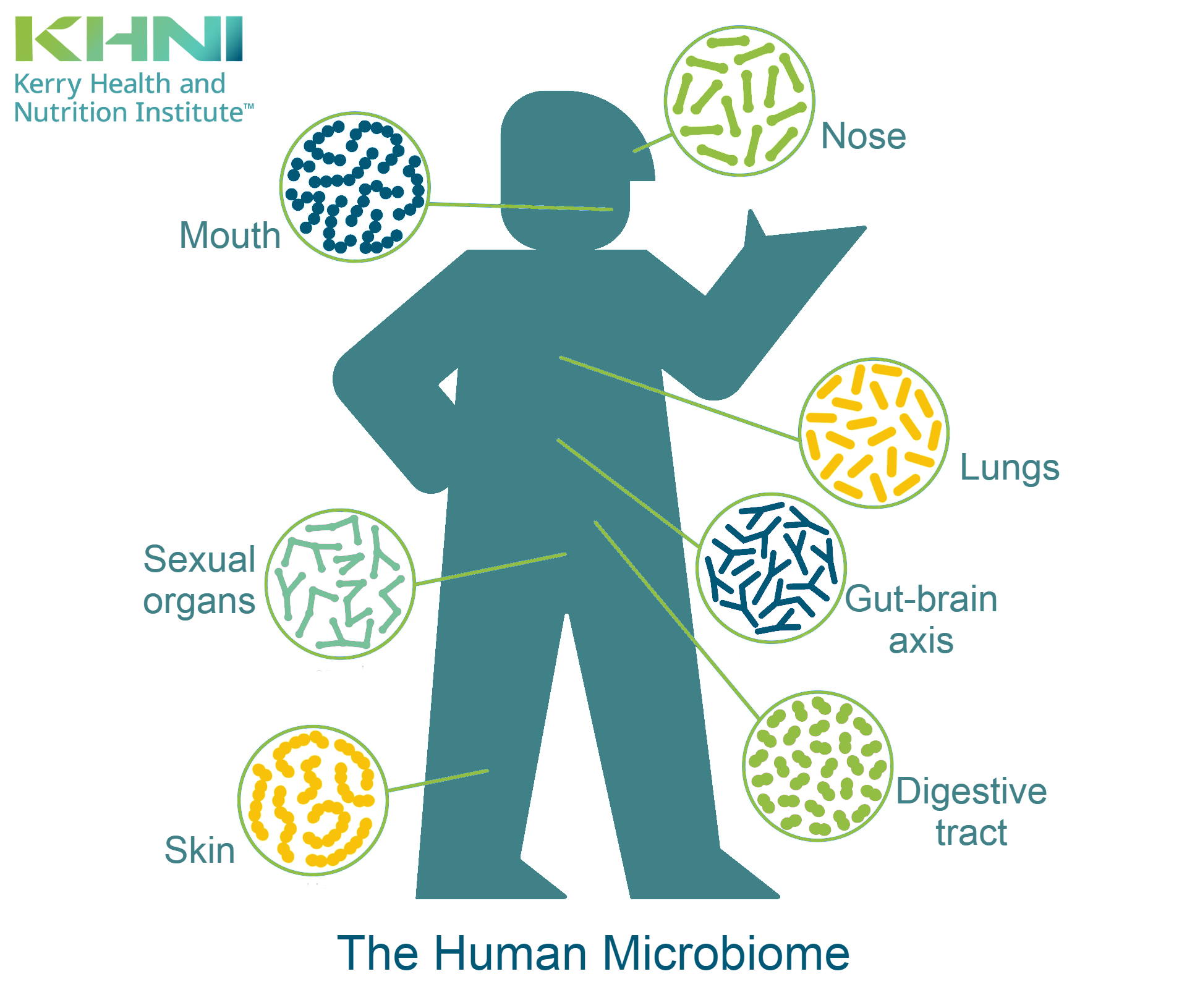
Gut bacteria and mood – the gut-brain axis
What is the Gut-Brain Connection?
The gut-brain connection refers to the relationship that the gut and its associated ecosystem has with the brain and nervous system. Specifically, the digestive system has its own nervous system (the enteric nervous system) which has more neurons than the spinal cord. This nervous system controls organs and muscles and allows the gut to operate semi-independently.
The enteric nervous system is connected to the central nervous system (brain and spinal cord) via the vagus nerve, which acts like a giant nerve superhighway that carries nerve transmissions to and from the brain. Thinking of a highway, picture what it looks like during rush hour. Typically, the flow of traffic is heavier going one way than the other. It carries more information from the gut to the brain than it does from the brain to the gut. This is why the term ‘second brain’ makes so much sense. It’s relaying just as much information about the state of the health, mood and well-being, as our ‘first’ brain.
The gut-brain axis and mental health
Research has now started to build out the connections between mental health, gut health, and the role of our microbiome, but there are far more questions than answers at this point.
Emerging evidence has shown that some probiotics can influence the level of the neurotransmitters serotonin and GABA (a neurotransmitter that promotes relaxation and reduces anxiety).
Locally in the gut, serotonin affects the motility of the gut, but there are hints that gut-produced serotonin may have an impact on the brain itself. Often called the ‘feel good hormone,’ serotonin acts as both a hormone and a neurotransmitter in our body. Low mood, depression, and anxiety can be associated with altered serotonin levels. For all of its importance to mental wellbeing, you might expect that the brain is where we find most of the body’s serotonin, but it’s not. In fact, the gut contains the vast majority of the serotonin in our body.
-
- Learn more: Serotonin: The Happy Hormone Produced In Our Gut
Microbiome and the immune system
How does the microbiome influence the immune system?
The microbiome is necessary for the normal development of a healthy immune system. Research in animal models has shown that an immune system that develops without exposure to a microbiome is ineffectual and dysregulated. The importance of immunity in the gut is likely because the gut contains the highest concentration of microorganisms in contact with immune tissue in our body, so we must protect ourselves from invasion of harmful pathogens entering the body through the gut.
In the gut, our immune system has direction interaction with pieces of bacteria, viruses, and yeasts/fungi that make up the gut microbiome. The interaction between the gut microbiome and the immune system is extremely complex and involves not just the microbes themselves but also metabolites that are created by the normal life processes of the microbes and released into contact with our cells and tissues.
These microbes provide examples of MAMPs (microbe-associated molecular patterns). By collecting data on the variety of MAMPs in the microbiome, our immune system becomes more readily able to defend the body against microbes that could result in harm to the body. Think of it as a sort of microbial surveillance system that our immune system learns and adapts from.
Examples of categories of microbes the immune system has to handle are RNA viruses (like influenza or SARS-CoV-2, DNA viruses (like smallpox), lipopolysaccharide-containing bacteria (like E. coli), peptidoglycan-containing bacteria (like Staph or Strep bacteria).
How do probiotics impact immunity?
A 2015 Cochrane Review titled Probiotics for Preventing Acute Upper Respiratory Tract Infections, which included 13 randomized controlled trials, found that probiotics were significantly better than placebo for reducing the number and duration of upper respiratory tract infections. This means that probiotics are likely working with the immune system to have a protective effect against the pathogens that cause URTIs.
The authors of the 2015 Cochrane Review suggest probiotics can influence immunity in the following ways:
-
- Probiotics have been shown to help protect against infection by improving the strength of the intestinal barrier between the inside of the intestine and our body. This reduces the ability of infectious microbes to enter our body via our gastrointestinal tract.
- Some probiotics can produce proteins or acids that inhibit the growth of pathogens in the GI tract
- Some probiotics, or the products they produce, can interact with the immune cells of the human body to influence their effectiveness (LPI, Cochrane). For example, some probiotics can increase the production of cytokines in the intestine. These cytokines act as chemical messengers to regulate immune responses.
Read Immunity Ingredients At-A-Glance: Probiotics to learn more
Learn more about the microbiome and immune health:
The vaginal microbiome and women’s health
 The vaginal microbiome refers to the billions of microorganisms that colonize in the vagina due to the moisture, nutrients, and temperature present. Most of the microorganisms in the vagina stem from the gastrointestinal tract and is mainly comprised of bacteria from the Lactobacillus genus. These microorganisms maintain a homeostasis relationship with their environment and allow the release of antimicrobial and anti-inflammatory compounds. The Lactobacillus genus produces several antimicrobial compounds, such as lactic acid, hydrogen peroxide (H2O2) and bacteriocins. These compounds make it possible to create a solid line of defense against certain pathogens to protect against infection. The regulation of the pH is also due in part thanks to the release of lactic acid by the Lactobacillus bacteria.
The vaginal microbiome refers to the billions of microorganisms that colonize in the vagina due to the moisture, nutrients, and temperature present. Most of the microorganisms in the vagina stem from the gastrointestinal tract and is mainly comprised of bacteria from the Lactobacillus genus. These microorganisms maintain a homeostasis relationship with their environment and allow the release of antimicrobial and anti-inflammatory compounds. The Lactobacillus genus produces several antimicrobial compounds, such as lactic acid, hydrogen peroxide (H2O2) and bacteriocins. These compounds make it possible to create a solid line of defense against certain pathogens to protect against infection. The regulation of the pH is also due in part thanks to the release of lactic acid by the Lactobacillus bacteria.
What disrupts the vaginal microbiome?
The balance maintained by microorganisms in the vagina can easily be disturbed by various internal or external factors. These internal factors include hormonal fluctuation that exists over a woman’s lifetime, age, immune system, and changes in the host’s environment. Other external factors can also disrupt this fragile ecosystem such as antibiotic therapy, infections, exposure to different microbes and an active sex life.
The vaginal microbiome and UTIs (urinary tract infections)
Urinary Tract Infections (UTIs) are common in women. It is usually caused by bacteria naturally present in the intestine, for example Escherichia coli, the main bacteria responsible for UTIs, which passes from the rectum to the urethra and ends up in the urinary tract. The elderly can be at higher risk for UTIs due to factors like diet or fluid intake, obstruction, etc. Lactobacillus bacteria, which mainly colonize the urogenital system, allow, among other things, the release of lactic acid, interfering with the adhesion of E. coli by downregulating some virulence factor expressions. This explanation would make it possible to use Lactobacilli as a possible solution to manage the recurrences of urinary tract infections.
The infant microbiome
When and how is a baby’s microbiome developed?
 A baby’s gut microbiome is in constant development and linked directly to the mother’s microbiome through pregnancy, delivery, and breastfeeding. It was long believed that the fetus remained sterile or almost until delivery, but this is now challenged by studies identifying bacteria, bacterial DNA, or bacterial products in meconium, amniotic fluid, and the placenta; indicating the initiation of maternal-to-offspring microbial colonisation in utero.
A baby’s gut microbiome is in constant development and linked directly to the mother’s microbiome through pregnancy, delivery, and breastfeeding. It was long believed that the fetus remained sterile or almost until delivery, but this is now challenged by studies identifying bacteria, bacterial DNA, or bacterial products in meconium, amniotic fluid, and the placenta; indicating the initiation of maternal-to-offspring microbial colonisation in utero.
Many factors will have an impact on the development of the gut microbiome after birth. These factors include age, diet, host genetics, antibiotic usage, mode of birth, type of feeding (i.e., breast milk or formula milk), and the birth environment of the infants (e.g., NICU). The mode of birth determines how the baby’s gut microbiome will be colonized and by which microorganisms. For the infant, a natural birth will typically lead to colonisation by the mother’s birth canal, making the baby’s microbiome is then similar to the one of the mother. On the other hand, babies born by C-section typically have a gut microbiome that more closely resembles the microbiome of the mother’s skin. In addition, C-section’s baby have a higher chance to acquire atopic diseases during the first two years after birth.
How does breastfeeding affect the infant microbiome?
The most plausible explanation is that it’s possible for the mother’s gut microbiome to be translocated towards mammary glands. Certain immunity cells can sample live commensal bacteria from the gut lumen and keep them in the mesenteric lymph nodes. From there, the bacteria can circulate to other locations in the body, including the mammary glands.
Some components from breast milk such as Human Milk Oligosaccharides(HMOs), Secretory IgA, Antimicrobial Proteins and Peptides, Tryptophan Metabolites and Lipids can also have an impact on the gut microbiome of the baby. The scientific literature is still developing on all the possibilities to modulate breastmilk factors involved in the microbiota shaping2.
Improving the gut microbiome with diet
Many factors may affect positively or negatively the gut microbiota. Dietary composition and habits are the most impactful factors modulating the dynamic gut microbiota. The main compounds included in the diet such as proteins, carbohydrates, fats or also fibers certainly have an impact on the gut microbiota and on the overall health. Certain diets that are less favorable to a diversified intestinal microbiota can actually cause dysbiosis within this ecosystem and even trigger a pro-inflammatory process.
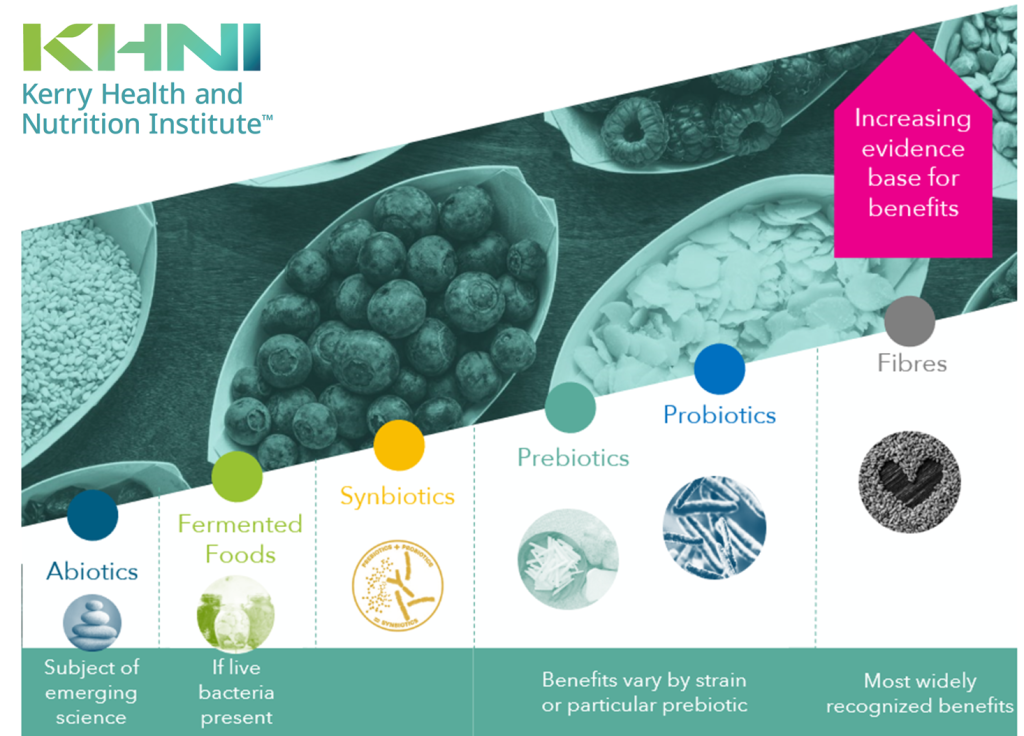
The strength of evidence for different ways we can improve our digestive health is constantly changing, but generally we know that fibre and probiotics are the most well-supported
Fibre, carbohydrates, and prebiotics
Fibres are necessary for optimal intestinal health through increasing stool volume, regulation of transit time to improve nutrient digestion and absorption. Some fibres can be used as fuel by microbes in our microbiome. The term prebiotic is used to describe these types of components in food. The result of this fermentation allows the production, by certain bacteria, of the famous short-chain fatty acids (SCFAs). Propionate, acetate, and butyrate are three short chain fatty acids and due to their low pH, inhibit the growth of pathogenic bacteria. These SCFAs also improve the integrity of the intestinal barrier while having anti-inflammatory effects and influencing the production of certain neurotransmitters such as serotonin. Common prebiotics include: Fructo-oligosaccarides (FOS) or fructans and Galacto-oligosaccarides (GOS). Inulin is one of the most commonly used types of FOS found in few vegetables such as garlic, onions, banana, also in whole grains such as barley, rye and finally in roots like chicory roots. GOS are found in fermented dairy products such as yogurt, kefir and even in breast milk.
Consumption of microbes or their components – probiotics, postbiotics, and fermented foods
Direct consumption of microbes on the surfaces of foods we eat, living in fermented foods, or supplemented into foods or beverages can impact the microbiome. The most common way most people might know about this is through foodbourne illness – when we consume a pathogenic bacteria like E. coli, it can colonize in our body to cause an infection and illness. However, we can also consume beneficial microbes that can colonize in our body or benefit the microbiome in other ways through metabolites it produces, for example. Probiotics, fermented foods, and postbiotics are a few ways dietary microbes can have an impact on the microbiome.
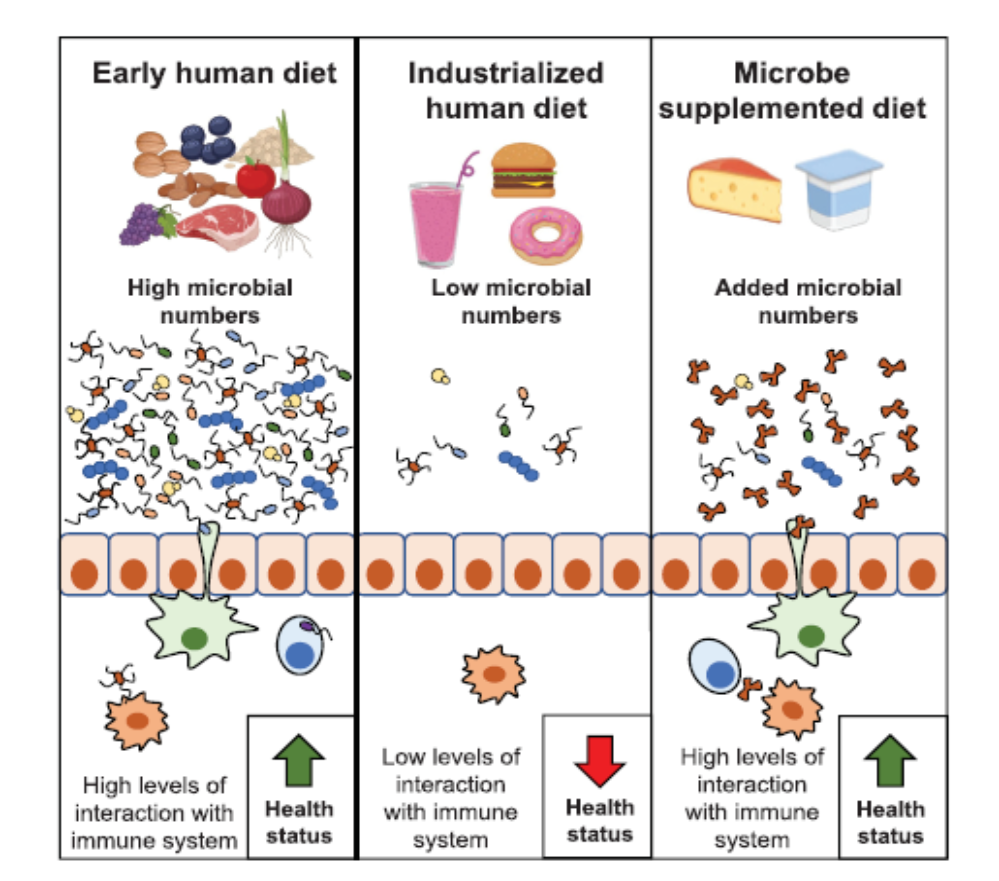
The hygiene hypothesis proposes that lower exposure to dietary microbes is linked to increased risk of some immune and metabolic diseases. Source: Marco et al 2020 J Nutrition